POMC deficiency, PCSK1 deficiency, and LEPR deficiency are rare genetic diseases of obesity
Genetic variants in the melanocortin-4 receptor (MC4R) pathway can impair the regulation of hunger, food intake, satiety, and energy expenditure.1,2
Impaired MC4R signalling can lead to hyperphagia (pathological, insatiable hunger) and early-onset, severe obesity, regardless of environmental and lifestyle factors.3,4
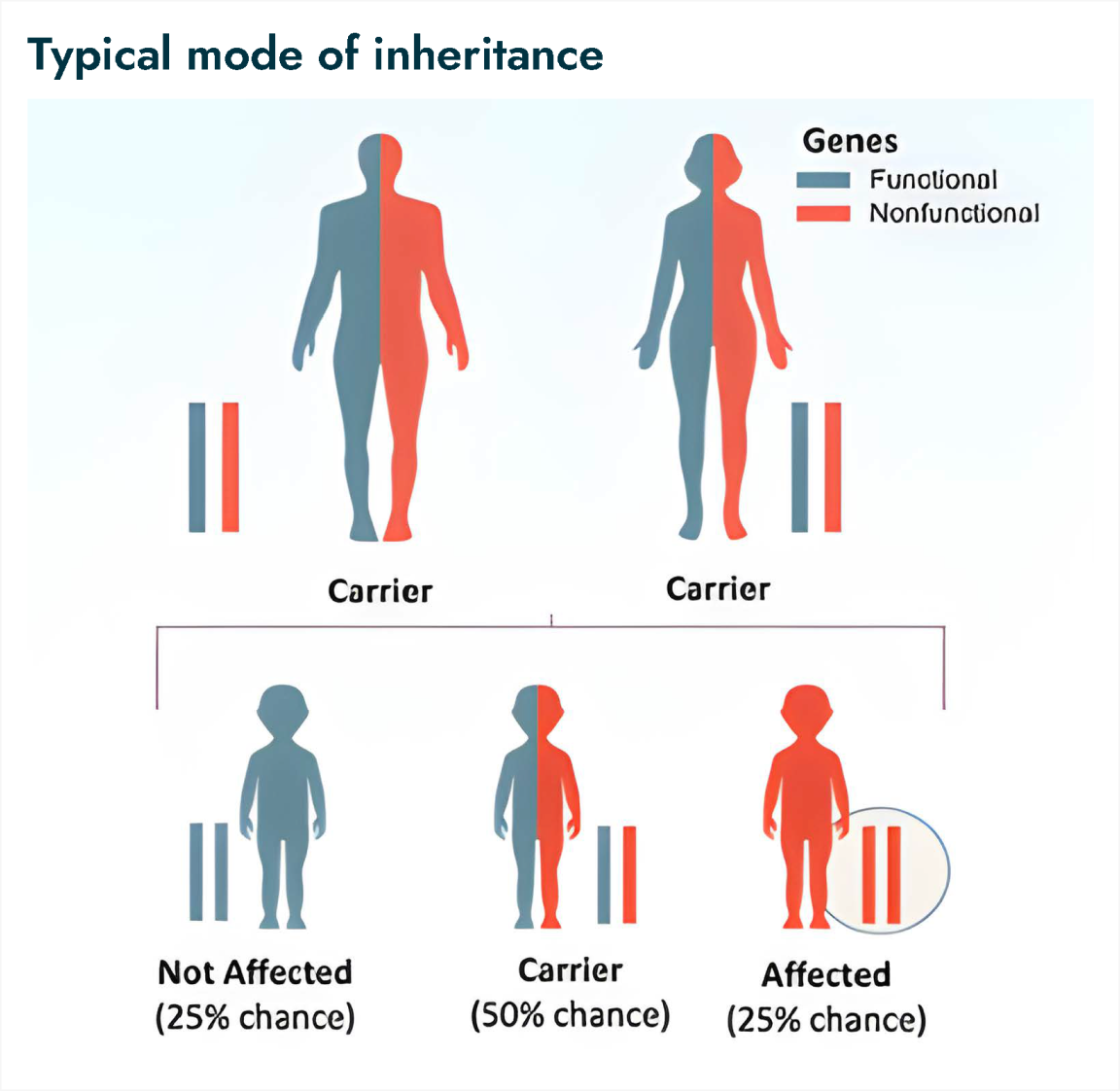
Pro-opiomelanocortin (POMC) deficiency, proprotein convertase subtilisin/kexin type 1 (PCSK1) deficiency, and leptin receptor (LEPR) deficiency are autosomal recessive inherited disorders caused by variants of the POMC gene, PCSK1 gene, and LEPR gene, respectively.4,5
| Key Clinical Features | POMC Deficiency6-9 |
PCSK1 Deficiency6,10,11 | LEPR Deficiency6,12,13 |
|---|---|---|---|
|
|||
| Other Potential Clinical Characteristics |
|
|
|
POMC, pro-opiomelanocortin; PCSK1, proprotein convertase subtilisin/kexin type 1; LEPR, leptin receptor.
Genetic testing is necessary to confirm diagnosis
POMC, PCSK1, and LEPR deficiencies are monogenic and require genetic testing to confirm diagnosis.14 They are also autosomal recessive diseases, so affected individuals have a variant in both copies of the gene.14
References:
1. Yazdi FT et al. PeerJ. 2015;3:e856. 2. Acosta A et al. Genes Nutr. 2014;9:384. 3. Haqq AM et al. Lancet Diabetes Endocrinol. 2022;10:859-868. 4. Huvenne H et al. Obes Facts. 2016;9:158-173. 5. Fonseca ACP et al. Obes Facts. 2016;9:158-173. 6. Styne DM et al. J Clin Endocrinol Metab. 2017;102(3):709-757. 7. Coll AP et al. J Clin Endocrinol Metab. 2004;89(6):2557-2562. 8. Mendiratta MS et al. Int J Pediatr Endocrinol. 2011;2011(1):5. 9. Argente J et al. Endocr Abstr. 2019;63:P976. 10. Stijnen P et al. Endocr Rev. 2016;37(4):347-371. 11. Martin MG et al. Gastroenterology. 2013;145(1):138-148. 12. Farooqi IS, O’Rahilly S. J Endocrinol. 2014;223(1):T63-T70. 13. Thaker VV. Adolesc Med State Art Rev. 2017;28(2):379-405. 14. Online Mendelian Inheritance in Man. Entries 609734, 600955, and 614963. https://www.omim.org/.
Accessed November 18, 2021.
